Cognitive behavioral therapy (CBT) and dialectical behavior therapy (DBT) are two popular psychotherapeutic modalities used for treating variety of mental health ailments. Through both CBT and DBT an individual will work with a mental health professional to learn how to process, cope with, and integrate challenging experiences as well as cultivate coping mechanisms, and helpful skills to effectively manage future challenges when they arise. DBT is a modified form of CBT, but its approach to treatment is distinct enough from CBT that the two models are considered unique. To recognize the difference between CBT and DBT it is helpful to gain a basic understanding of these two stand-alone therapeutic modalities.
Cognitive Behavioral Therapy
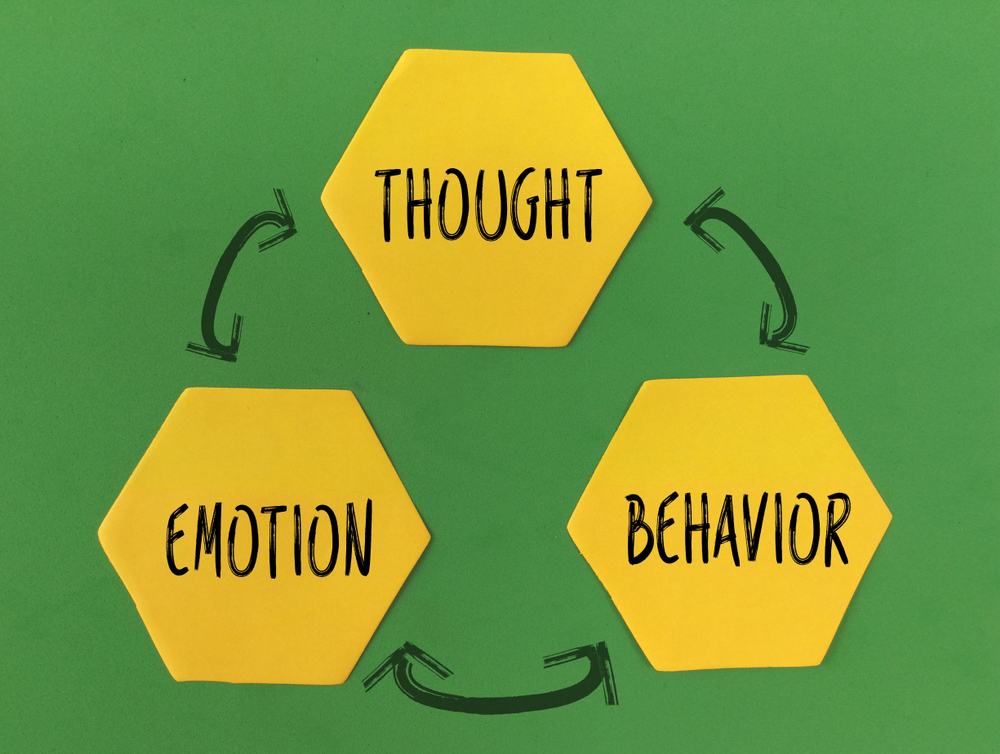
Cognitive behavioral therapy was developed in the 1960s by psychiatrist, Aaron Beck. It is a structured, short-term, goal-oriented form of psychotherapy. CBT is based on the notion that thoughts and behaviors influence feelings; therefore, shifting the way one thinks and reacts to situations can subsequently improve one’s emotional demeanor. Cognitive behavioral therapy focuses on specific problems and utilizes a goal-oriented approach. In CBT, a therapist will encourage his or her client to discuss his or her troubling thoughts and/ or feelings. The steps of CBT include the following, provided by Psychology Today:
- Identify troubling situations and/ or conditions in your life (e.g., divorce, a medical condition, anger, grief, etc.).
- Become aware of your emotions, thoughts, and beliefs connected to these troubling situations.
- Identify inaccurate and/ or negative thinking that may be contributing to your troubles.
- Reshape inaccurate and/ or negative thinking. To help facilitate this step, a therapist may encourage you to ask yourself if your view of the situation is based off an inaccurate perception of the situation or off facts.
The way CBT works is that through therapy, an individual will learn to understand that the way they behave has a direct correlation with their personal attitudes and emotional problems. Depending on the needs of the individual, the number of CBT sessions range from five to twenty sessions.
Dialectical Behavior Therapy
Dialectical behavior therapy is an evidenced-based, multifaceted, rigidly structured psychotherapy approach. It was developed in the late 1980s by Marsha M. Linehan, who was at the time a psychology/ suicide researcher at the University of Washington, as a means to help better treat chronically suicidal individuals diagnosed with borderline personality disorder (BPD). Psychology Today explains that the “goal of DBT is to transform negative thinking patterns and destructive behaviors into positive outcomes.” DBT employs many of the same components of CBT and combines concepts derived from Buddhist meditative practice such as awareness, mindfulness, and attentiveness to current situations and emotional experiences to encourage acceptance.
Dialectical behavior focuses on teaching behavioral skills in four key areas, called the four modules of DBT, which are: core mindfulness (focusing skills), distress tolerance (crisis survival skills), emotion regulation (de-escalation skills), and interpersonal effectiveness (social/ relationship skills). DBT is conducted in three different therapeutic settings: weekly individual therapy sessions, weekly DBT skills training group therapy sessions, and as-needed phone coaching between sessions. The full DBT program is intended to take twenty-four weeks to complete, as six weeks are allocated to focusing on each of the four DBT skills modules.
Differences
Aside from the differences in duration and format (e.g., unlike CBT, DBT has a group therapy component), the most noteworthy difference between these two modalities is the kind of change they impart. CBT focuses on rationale and reasoning (how thoughts, feelings, and behavior influence one another) to help individuals recognize and change problematic patterns of thinking and behaving. Whereas DBT emphasizes mindfulness practices, emotion regulation, and learning to tolerate pain through validation, acceptance, and behavior change to improve interpersonal relationships. CBT aims to provide individuals with the ability to identify damaging thoughts and teaches an individual how to redirect those thoughts. In DBT there is some emphasis placed on dealing with and navigating thoughts, however the primary focus of DBT is placed on helping individuals learn to identify triggers outside of themselves and pair those triggers with healthy responses and coping mechanisms.
The information above is provided for the use of informational purposes only. The above content is not to be substituted for professional advice, diagnosis, or treatment, as in no way is it intended as an attempt to practice medicine, give specific medical advice, including, without limitation, advice concerning the topic of mental health. As such, please do not use any material provided above to disregard professional advice or delay seeking treatment.